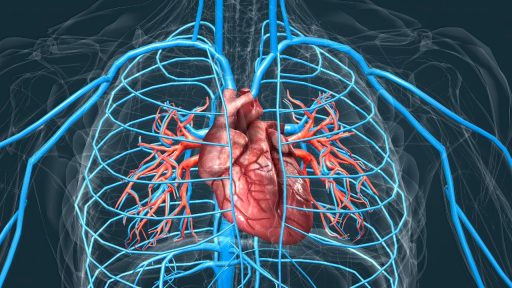
For generations, cardiology textbooks taught that once the heart was badly damaged, the loss was permanent. Today, a wave of research is overturning that dogma, revealing that the human heart carries dormant repair programs that can be switched back on. Scientists are not only mapping those self-healing circuits, they are beginning to harness them in ways that could change how heart attacks and heart failure are treated.
I see a clear throughline in the latest findings: from genes that coax adult heart cells to divide again, to stem cell patches that quietly rebuild scarred muscle, to evidence that failing hearts already attempt their own rescue. Together, these discoveries amount to compelling proof that the heart is not a passive victim of injury but an organ with a surprising capacity to regenerate when given the right signals.
From “fixed pump” to living, repairable tissue
Cardiologists long regarded the heart as a finished product by adulthood, a view summed up in the idea that it was a “post-mitotic organ” that could not regenerate. That assumption shaped decades of care, where treatment focused on limiting damage and managing symptoms rather than restoring lost muscle, a strategy reflected in analyses that note how therapy historically centered on “damage control” after injury rather than true repair, as outlined in Therefore. Even when patients survived major heart attacks, they were often left with a weakened pump and a lifetime of medications, because clinicians believed dead heart muscle could not come back.
Over roughly the past decade, that certainty has eroded as researchers have documented low but real turnover of heart cells in adults and identified multiple pathways for cardiac repair. A detailed review of these mechanisms describes “remarkable progress” since the first challenges to the old view, charting how scientists have uncovered resident stem cells, cell cycle regulators, and immune signals that all contribute to healing, in contrast to the earlier belief that the heart was an immutable organ, as summarized in Summary Remarkable. Clinicians who once repeated that the heart “cannot repair itself” now acknowledge that this was an oversimplification, a shift captured by cardiologist Ronen Beeri, who has described how the field is pivoting from resignation to regeneration.
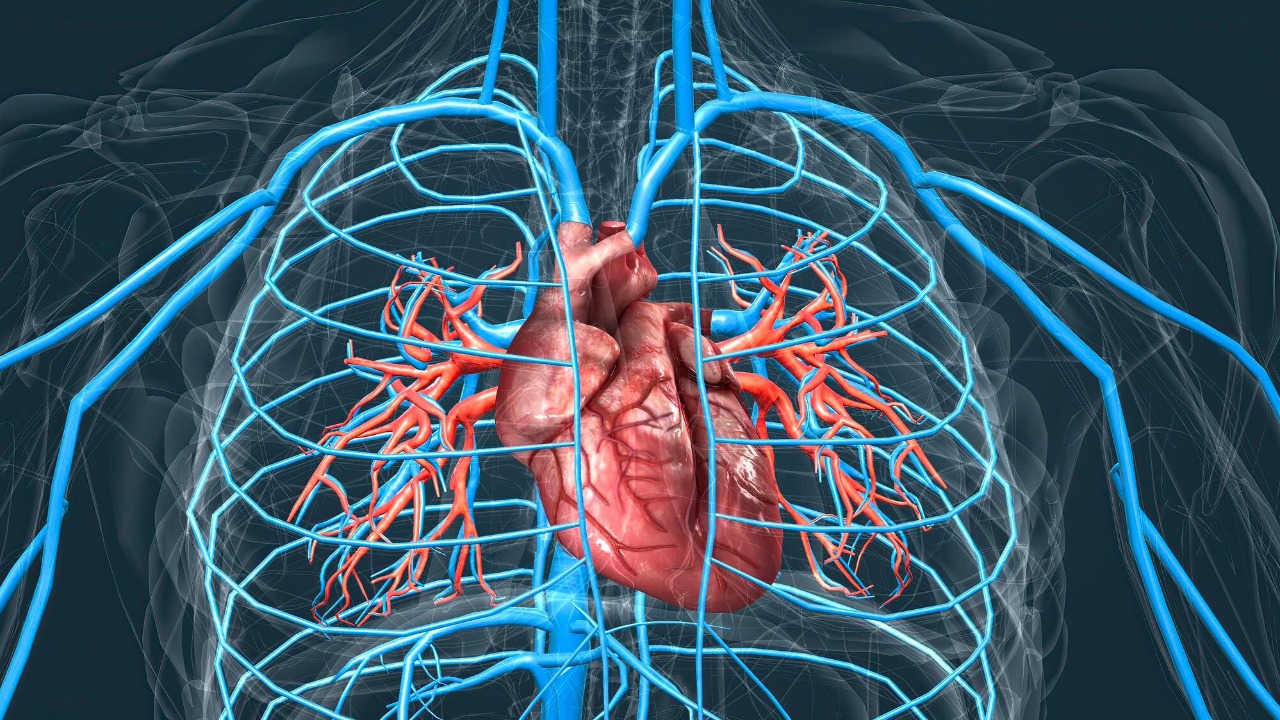
A hidden self-repair program inside failing hearts
One of the most striking developments is the realization that diseased hearts already try to heal themselves, even in advanced failure. Researchers examining tissue from patients with severe heart failure have found that the machinery for cell division is not completely silent; instead, certain molecular pathways are more active than in healthy hearts, suggesting an intrinsic attempt at regeneration that simply does not go far enough. In one investigation, scientists reported that markers of cell cycle activity were higher in failing hearts, and argued that this latent repair mechanism could be “kick-started” and boosted, a conclusion highlighted in work on a previously unrecognized regenerative capacity, as described in After.
Parallel work has reinforced that message by showing that the heart’s ability to regenerate is governed by specific molecular switches that can, in principle, be targeted. A report on a “self-healing” heart model notes that manipulating the pathways that control cardiomyocyte division could enhance the organ’s natural capacity to replace damaged cells, pointing to a future in which drugs or gene therapies nudge the heart back into a more youthful, regenerative state, as outlined in Findi. Even popular explainers now grapple with the question “can heart heal itself,” reflecting how far the conversation has moved from flat denial to nuanced exploration, as seen in a medical briefing that walks through these mechanisms in accessible language in Dec.
The gene that turns adult heart cells back on
The most headline-grabbing evidence that the heart can be coaxed into repair comes from work on a single gene that appears to act like a master switch for regeneration. At Mount Sinai, cardiologist and researcher Hina Chaudhry has focused on a naturally occurring gene called CCNA2, which regulates the cell cycle. Her team has shown that reactivating CCNA2 in adult heart cells can push them to divide again, effectively reversing the long-held assumption that mature cardiomyocytes are permanently locked out of replication. In preclinical models of heart attack and heart failure, delivering this gene reduced scarring and improved pumping function, suggesting a path to less invasive treatments that work with the heart’s own biology.
Follow-up work has underscored how targeted this effect can be. In one study, scientists reported that CCNA2 therapy triggered robust changes in diseased heart cells, while cells from a 21-year-old heart showed no response, implying that the intervention selectively benefits damaged tissue rather than indiscriminately forcing all cells to divide, a key safety signal described in Conversely. Coverage of this work has emphasized that a naturally occurring gene, rather than an artificial construct, is driving the effect, raising the prospect that therapies could amplify a process the body already uses, as detailed in reports on a specific human gene that can help the heart repair itself from heart attack or heart failure in Untitled.
Public-facing explainers have picked up on this theme, noting that scientists have found evidence that “Your heart will not just give you fear” but can mount a regeneration process in human samples when the right genetic levers are pulled. That framing, which highlights how a “New gene discovery” could help repair heart damage from heart attack or heart failure, captures the shift from fatalism to possibility that I see across the field, as summarized in New and echoed in a companion overview that stresses how Your own biology can be harnessed.
Stem cell patches and lab-grown tissue that quietly rebuild the heart
Genes are only one side of the story. Another line of research is trying to give the heart fresh building blocks in the form of stem cells and engineered tissue. In PHOENIX, a team of Mayo researchers has developed a patch seeded with stem cells that can be laid over damaged heart muscle, where it gradually releases cells and healing factors into the injured area. The design is meant to “gently heal” rather than overwhelm the tissue, addressing past concerns that injected cells often died or triggered arrhythmias. Early descriptions emphasize that the patch is intended for minimally invasive delivery, potentially sparing patients from open-heart surgery, as outlined in a detailed report on a new stem cell patch to heal damaged hearts in Untitled.
Separate coverage of the same platform underscores that the “beauty of this design” is its ability to restore function without major surgery, describing how Mayo Clinic scientists created a stem cell patch that aims to replace what is lost and help the heart beat more strongly, as explained in Mayo Clinic and in a related summary of how Nov innovations could heal hearts without surgery. Social media posts from the same institution describe how Researchers at the Mayo Clinic have also grown heart tissue from stem cells in the lab and used it to repair damaged hearts, positioning these approaches as part of a broader #HeartHealth and #RegenerativeMedicine push, as highlighted in a discussion of how the Mayo Clinic is tackling heart attack recovery.