Some people breeze through infections with barely a sniffle while others end up in intensive care, even when they face the same virus. For years that gap was blamed mostly on “good” or “bad” genes, as if DNA alone wrote each person’s fate. A different picture is now emerging from recent research, one where early immune reactions, life history and even the way viral debris attacks our cells can matter as much as inherited traits.
Scientists are beginning to map how those pieces fit together into a single story about who gets very sick and who recovers quickly. Their work points to a new idea: the real risk lies in how our immune system is wired, trained and sometimes sabotaged across a lifetime, not just in the sequence of letters in our genome.
How life experience rewrites the immune system
The latest data show a striking shift from blaming fixed genes to examining how life experience reshapes immune cells over time. Researchers at the Salk Institute have built an epigenetic catalog that tracks how inherited traits and lived events both leave marks on the immune system. They found that stable, hard coded regions of DNA carry the basic blueprint, while flexible regulatory stretches act like switches that can be flipped by infection, stress or environment, changing how immune cells behave without altering the underlying sequence.
One report explains that these experience driven changes cluster in regulatory regions that function as molecular dimmer switches, raising or lowering the activity of key immune genes in the very cells where disease begins. The work, led by Researchers at the, shows how nature and nurture combine inside T cells, B cells and other defenders, which helps explain why two people with similar DNA can respond so differently to the same pathogen.
Beyond genes: why some immune systems overreact
This epigenetic wiring is increasingly seen as the missing link between raw genetics and real world illness. A recent analysis framed it bluntly, arguing that it is not just genes that determine who gets sicker but also how those regulatory switches have been tuned across a lifetime. The piece describes how early infections, chronic stress and environmental exposures can leave chemical marks on immune DNA, shifting the balance between helpful inflammation and damaging overreaction when a new virus appears.
In that work, the authors highlight how these flexible regions act as a mechanism that explains disparities in disease severity that simple genetic testing cannot. They describe how life experiences concentrate changes in those regulatory switches, which can prime some people for a faster, more controlled response and leave others vulnerable to runaway inflammation. That argument, laid out in detail in a recent report, lines up with the Salk team’s epigenetic catalog and helps connect molecular biology to the everyday reality of who ends up in a hospital bed.
The nose as an early battleground
Even before those deeper epigenetic patterns kick in, another key difference emerges right at the body’s front door. Work on the common cold shows that the first line of defense sits in the nose, where epithelial cells coordinate an early antiviral response. Using a detailed model of rhinovirus infection, scientists watched thousands of individual cells and saw that some people’s nasal tissue launches a rapid wave of interferons, the signaling proteins that warn neighboring cells and slow viral spread, while others lag behind.
That lag can be the difference between a mild cold and a serious illness. The researchers describe how strong early production of interferons and other antiviral molecules in nasal cells limits the virus before it gains a foothold deeper in the airways. Their findings, which focus on Interferons and Early a sophisticated single cell model, match broader observations that some people’s first immune wave is both faster and better coordinated, which keeps symptoms mild even when they carry the same viral load as a sicker neighbor.
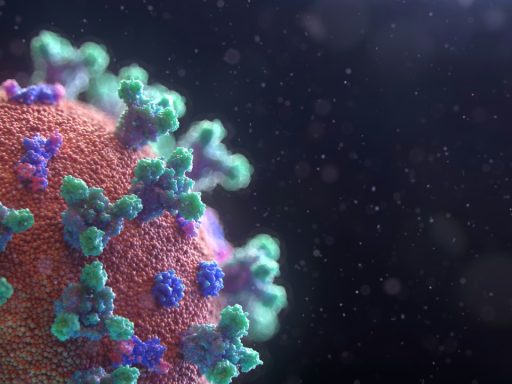
When the virus fights back against immunity
Genetics and early response only tell part of the story, because viruses also manipulate the immune system from the inside. A UCLA led team has shown that when human enzymes chop up the spike protein of the virus behind COVID 19, some of the resulting fragments can target and kill specific immune cells. That amounts to a kind of molecular sabotage, where the very process of breaking down the virus creates pieces that then damage the body’s own defenders.
The researchers describe how these fragments affect different immune cell types and may help explain why certain variants cause more severe disease than others. Their findings on COVID 19 viral also offer clues about why some versions of the virus, such as omicron, spread easily but tend to produce milder symptoms, because the pattern of fragments and the cells they hit appears to shift between variants.
Why the same exposure can mean no symptoms at all
At the far end of this spectrum sit people who never feel sick even when lab tests show they are infected. Genetic work on SARS CoV 2 has identified one such factor, a variant in the HLA B gene that seems to give carriers a head start. According to one study, this version of HLA B does not prevent infection with SARS CoV 2 but helps T cells recognize the virus more quickly, so the immune system clears it before symptoms appear.
The lead author, geneticist Danillo Augusto, explains that people with this HLA B variant can still carry and transmit the virus, yet their internal response is so fast that they never experience the fever, cough or fatigue that send others to bed. The report on The HLA variant estimates that roughly one in five infected people may fall into this asymptomatic group, which shows how a single gene can still tilt the odds even in a story dominated by epigenetics and environment.