A newly identified virus hiding inside a common gut bacterium is emerging as a potential driver of colorectal cancer, one of the world’s deadliest malignancies. The discovery links a microscopic parasite of bacteria to tumors in the human bowel and raises urgent questions about how infections might quietly set cancer in motion years before symptoms appear.
Researchers now report that this virus shows up far more often in people with colorectal cancer than in healthy individuals, and that its presence may help explain puzzling patterns seen in the gut microbiome of patients. The finding could open a path toward earlier detection and targeted prevention, although scientists caution that the work is still at an early stage.
Inside the study that exposed a hidden viral suspect
The new work grew out of a longstanding mystery around a bacterium called Bacteroides fragilis, one of the most common microbes in the human intestine yet repeatedly linked to colorectal tumors. Researchers from the University of Southern Denmark and collaborators set out to understand why this familiar organism seemed to appear more frequently in patients with bowel cancer than in healthy controls. By analyzing tumor samples and stool from large patient cohorts, they found that a specific virus infecting Bacteroides fragilis appeared far more often in people with colorectal cancer than in those without, according to a detailed summary of the investigation.
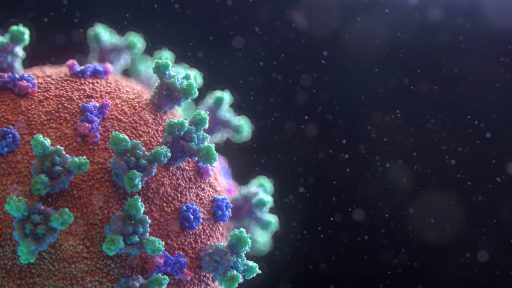
The virus is what scientists call a prophage, meaning it embeds its genetic material inside the DNA of its bacterial host and can sit there quietly for long periods. In this case, the prophage was found integrated in Bacteroides fragilis strains that were enriched in colorectal cancer tissue, suggesting a tight ecological relationship between the virus, the bacterium, and the tumor environment. The group, led by Flemming Damgaard, reported that in patients who later developed colorectal cancer, this prophage-carrying Bacteroides fragilis could already be detected in earlier stool samples, hinting that the infection might precede and possibly promote the disease, as described in a report on the newly linked virus.
How a common gut bacterium became a cancer hot spot
Bacteroides fragilis has long been viewed as a double-edged resident of the gut, essential for breaking down complex carbohydrates yet also implicated in inflammatory conditions and colorectal tumors. The bacterium is part of the normal microbiota that colonizes the body, and it can be found in the intestines of the vast majority of healthy individuals, according to a background explainer on Bacteroides fragilis. For several years, oncologists and microbiologists have noticed that certain strains of this species, especially those that produce toxins, show up repeatedly in tissue from colorectal cancer patients.
The new research suggests that the virus inside these bacteria may be a key reason why some strains behave differently from others. When the prophage infects Bacteroides fragilis, it can change the bacterium’s genetic profile and potentially alter how it interacts with the intestinal lining. Scientists involved in the project report that the virus-positive strains were more common in tumor tissue than in nearby noncancerous sections of the colon, and that they appeared more frequently in patients with cancer than in control groups that remained healthy, according to the large datasets summarized in a research briefing.
What the virus actually does inside tumors
At the molecular level, the newly described prophage appears to reshape the bacterial community that lives in and around colorectal tumors. A detailed analysis of tumor-associated microbiomes found that colorectal cancer tissue is enriched with distinct prophage infections, including this previously unknown virus, compared with healthy colon samples. In particular, the study showed that colorectal cancer is linked to specific patterns of viral DNA integrated into bacterial genomes, suggesting that these infections are not random but instead track closely with disease status, according to the authors of a plain language summary of the findings.
One hypothesis is that the virus may boost the ability of Bacteroides fragilis to produce or deliver toxins that damage DNA in human cells, which could set the stage for cancerous mutations. Colorectal cancer, commonly called bowel cancer, has already been connected to a gut toxin that might help explain why more young adults are being diagnosed, according to scientists who have highlighted this generational shift in a widely shared discussion of early. The new virus-centered research fits into that broader picture by suggesting that infections inside bacteria may be one of the triggers that turn a common gut resident into a more dangerous, toxin-associated strain.
From correlation to risk: how strong is the cancer link?
Although the virus appears more frequently in patients with colorectal cancer than in healthy controls, researchers are careful to stress that correlation does not yet prove causation. Current data show that virus-infected Bacteroides fragilis strains cluster in tumor tissue and that they can be detected in stool samples from people who later develop colorectal cancer, as described in the Communications Medicine paper. That pattern strongly suggests that the infection is associated with disease risk, but scientists still need to demonstrate exactly how the viral genes change bacterial behavior and whether blocking the virus can reduce tumor formation.
To move from association to proof of risk, the teams behind this work are turning to larger cohorts, animal models, and mechanistic experiments. They are examining whether the prophage carries genes that directly influence toxin production, immune evasion, or adhesion to the gut lining, and whether removing or inactivating the virus in Bacteroides fragilis reduces the bacterium’s ability to promote tumors. Earlier research into early onset colon cancer has already suggested that specific microbial toxins might be a driver of the alarming spike in cases among younger adults, according to scientists who described a potential new cause in an analysis of rising. The viral discovery adds another layer by pointing to a genetic switch inside the bacteria that could be responsible for turning that risk on.
What this could mean for screening, prevention, and treatment
If the association between the virus and colorectal cancer holds up in larger studies, it could reshape how clinicians think about screening and prevention. Because the prophage-infected Bacteroides fragilis strains can be detected in stool samples, one future possibility is a noninvasive test that flags people who carry the high-risk combination of bacterium and virus years before tumors appear. Researchers from the University of Southern Denmark have already highlighted that the virus is present in a vast majority of healthy individuals, according to their broader description of how the gut microbiota harbors both harmless and potentially dangerous strains. That ubiquity means any screening tool would need to distinguish between low-risk carriage and patterns that truly signal danger.
Therapeutically, the discovery opens the door to new strategies that target the virus, the bacterium, or both. One concept is to design bacteriophage-based therapies that selectively attack the high-risk Bacteroides fragilis strains, or to develop vaccines that prevent the prophage from integrating into the bacterial genome in the first place. Another path could involve small-molecule drugs that block key viral genes and blunt the bacterium’s ability to damage the intestinal lining. The original study, which appears in Communications Medicine, has already prompted calls for larger international datasets and long-term follow-up, so that clinicians can translate this basic science into practical tools for reducing colorectal cancer risk.